September 12, 2021, by mszrm4
Teaching clinical examination skills online: Will COVID change long term practice?
Dr Jay is an alumni of the Nottingham MedEd course and writes below about the the changes Covid brought to the clinical skills team at UoN
The Covid pandemic has caused considerable disruption to education across the globe and the education of healthcare professionals has been particularly affected, as so much learning occurs in a clinical context – usually with close contact between students, clinicians and patients [1]. The rapidly changing nature of the pandemic has been particularly difficult for educators, as they have had to make rapid and repeated changes as the situation evolves [1, 2].
This blog discusses some of the adaptions and challenges that the Nottingham clinical skills team have made to deliver early years clinical skills teaching during the pandemic, how it has been perceived by students and what changes will remain in the long term.
Historically:
Early years clinical skills teaching at Nottingham focused on providing students with a basic approach to systems examinations (such as the cardiovascular system) that they can learn to adapt as they progress through the course. This was delivered in face-to-face sessions where approximately 40 students received a presentation outlining the structure of the examination, a tutor demonstration, then a period of practice under supervision. Each session lasted around 2 hours. Additionally, students would have opportunities to attend hospital and GP placements to practice their skills in the clinical environment.
Changes due to Covid:
Covid meant that face-to-face contact needed to be rapidly reduced and students supported to learn from a variety of diverse locations rather than on campus. Staff were particularly concerned by a lack of supervised practice if online learning only was adopted. Small group tutorials online, with students demonstrating to a staff member, were considered but cohort size and the available staff time made this impossible. Staff therefore came up with a hybrid approach to delivering teaching using a flipped classroom approach:
- Existing teaching presentations were updated and turned into recorded, narrated online presentations that students were encouraged to access in advance of the session.
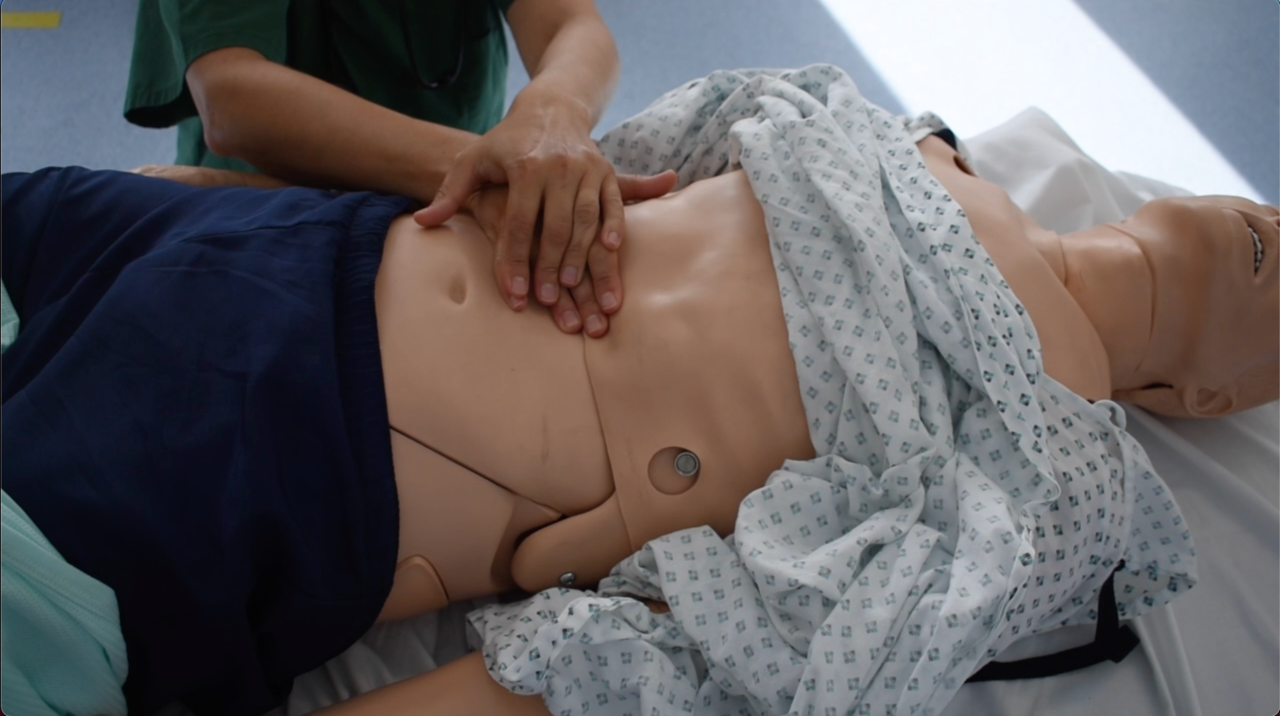
- Each of these presentations was accompanied by a short online video demonstration, filmed by staff. Films were created using best practice in instructional design for educational videos and put together with standard computer equipment available to staff [3]. An example of these is presented here: Video on how to test capillary blood glucose
- The recorded presentations and videos were made available to students several weeks before a synchronous online session delivered via Microsoft teams. In this session, the clinical skills team would provide live demonstrations via video from the clinical skills suite and then answer student’s questions with demonstrations to provide clarification. These sessions would usually involve three members of staff: one managing the technology, one demonstrating and a third one acting as curator and facilitating discussions.
- Finally, the students attended a shorter face-to-face session where they were offered the opportunity to practice in pairs in the clinical skills centre (with PPE and social distancing). This allowed staff to observe and provide feedback and support for students.
- Overall these sessions lasted slightly longer than the original 2-hour sessions students used to receive and the new sessions quite intensive on staff time.

Evaluation:
Evaluation was conducted while sessions were ongoing, initially as part of a review process to inform future sessions as part of an iterative process (rather than as a formal evaluation for publication). Students reported sessions as having an average score of 4.2 (on a 5-point Likert scale) for being relevant, useful, and interesting. Initially, high numbers of students (nearly 75%) reported technological difficulties with the online sessions. Moving from wireless to wired microphones and cameras reduced this to 7% by the end of the second semester, however by this point many students had returned to campus and were not having to rely on mobile or rural broadband.
Analysis of student performance in the end-of-year practical examinations did not show a decrease in performance compared to previous years. However, exams were run and administered differently to previous cohorts due to Covid precautions, which makes it difficult to make direct comparisons between this and previous years’ performances. A number of students reported that the face-to-face contact with staff made them feel supported and as though the faculty had investment in them as individuals, which they felt was particularly valuable for their education.
Whilst this was a rapidly evolving teaching plan with an informal evaluation, the results do suggest that this form of hybrid education is acceptable to students, at least (bearing in mind the limitations of social distancing) replicating the finding of previous work [4]. Anecdotally, staff felt that the flipped classroom approach had encouraged independent learning in students, which they were keen to maintain. As such, some of the changes made due to Covid will be kept, at least in the short term.

Future plans:
The team are looking at app-based video hosting options, as students seem to use their mobile devices to regularly engage with video and online content during practical sessions before seeking advice from tutors. However, there are significant concerns that – whilst some elements of skills teaching can be replaced by online sessions – other elements are more challenging, such as those involving social interactions and relationships.
The environment in which the learning takes place plays a significant role in learner development [5]. Equally, the reduction of contact with patients may limit the transfer of communication skills from the classroom to the clinical environment. Support and supervision and modelling from senior clinicians is key to the transfer of communication skills[6]. Perhaps staff have not addressed these elements in the recent rapidly evolving teaching and clinical environment seen over the last 18 months but, if online hybrid education is to continue into the future, staff will have to how to replicate or replace certain elements of clinical experience that may be lost in online teaching, or risk a negative impact on students’ futures.
Dr Robert Jay, MBChB, MRCGP, MMedSci, PGCert Clin Sci, MRCPathME, FHEA, is an Alumni of the Nottingham MedEd course. He currently works as a Medical Education Fellow in the Assessments Team and a Clinical Skills Teaching Fellow at the University of Nottingham.
Join us on the Nottingham MedEd course: https://www.nottingham.ac.uk/pgstudy/course/taught/medical-education-mmedsci
References:
1. Jeyakumar, Y., et al., Limitations in virtual clinical skills education for medical students during COVID-19. Canadian Medical Education Journal, 2020. 11(6): p. e165.
2. Sandars, J., et al., Twelve tips for rapidly migrating to online learning during the COVID-19 pandemic. MedEdPublish, 2020. 9.
3. Scientists, T.L. Designing Effective Instructional Videos. 2021 [cited 2021 22/08/21]; Available from: https://www.learningscientists.org/blog/2021/7/1-1.
4. Adam, M., et al., The Use of Short, Animated, Patient-Centered Springboard Videos to Underscore the Clinical Relevance of Preclinical Medical Student Education. Academic Medicine, 2017. 92(7): p. 961-965.
5. McKimm, J., K. Forrest, and J. Thistlethwaite, Medical education at a glance. 2017: John Wiley & Sons.
6. Brown, J., Transferring clinical communication skills from the classroom to the clinical environment: perceptions of a group of medical students in the United Kingdom. Academic Medicine, 2010. 85(6): p. 1052-1059.
No comments yet, fill out a comment to be the first

Leave a Reply