November 6, 2020, by School of Medicine
50 at 50: Sir Peter Rubin: Overcoming challenges and embracing opportunities
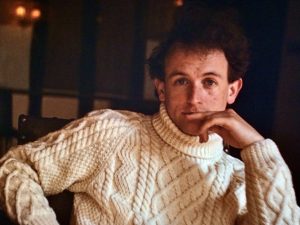
 Sir Peter Rubin was Professor of Therapeutics at Nottingham from 1987 – 2014 and Dean of the Faculty of Medicine and Health Sciences from 1997 – 2003. While at Nottingham, Sir Peter led a number of momentous developments within the Faculty, including the development of the Graduate Entry Medical School in Derby and the Nottingham Vet School. He was Chair of the General Medical Council from 2009 – 2014 and was knighted for services to medicine in 2010.
Sir Peter Rubin was Professor of Therapeutics at Nottingham from 1987 – 2014 and Dean of the Faculty of Medicine and Health Sciences from 1997 – 2003. While at Nottingham, Sir Peter led a number of momentous developments within the Faculty, including the development of the Graduate Entry Medical School in Derby and the Nottingham Vet School. He was Chair of the General Medical Council from 2009 – 2014 and was knighted for services to medicine in 2010.
In this blog, Sir Peter reflects on the trials and tribulations of his inspiring medical career – the highs and the lows – that in equal measure shaped the path to his success. It’s a lesson to us all in seeing opportunity in rejection and making the most of every moment presented to us.
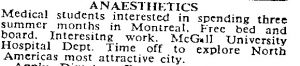 “If it hadn’t been for these few lines at the back of the BMJ I wouldn’t have gone to Montreal; I probably wouldn’t have become a Clinical Pharmacologist; and I almost certainly wouldn’t have felt quite so strongly about the importance of treating medical students and young doctors with fairness and respect.
“If it hadn’t been for these few lines at the back of the BMJ I wouldn’t have gone to Montreal; I probably wouldn’t have become a Clinical Pharmacologist; and I almost certainly wouldn’t have felt quite so strongly about the importance of treating medical students and young doctors with fairness and respect.
“And, later in my career, if I had been appointed to a post I really wanted at another university, I wouldn’t have spent many happy years as a professor at Nottingham and I wouldn’t have become Chair of the GMC. I had absolutely no interest in medical regulation. But back then medical schools took turns to nominate a Dean to the GMC; it happened to be Nottingham’s turn; I happened to be Dean. It was as random as that. And I eventually discovered that regulation can be interesting. Honestly – it really can!
“Careers can be as much about luck, seeing opportunities in rejection and making the most of wherever you find yourself as they are about talent, hard work and good role models, hugely important though these are.
 “But back to Montreal…I went in the long vacation after second year. I’d never been on a plane and it was a great adventure. I’d also never seen a patient and that was a bit of a problem because it turned out that “second year” in Canada meant something very different to what it meant in the UK. But my hosts were very generous and wanted to persuade medical students to choose anaesthesia as a career. I spent the summer in two intensive care units, one run by the anaesthetists and the other by clinical pharmacologists. I had enjoyed pharmacology the previous year and here it was in action: I loved it and I had some great mentors encouraging me to understand more. This early experience led eventually to my choice of career. I also loved Montreal and I went back for some of my later clinical attachments, including Paediatrics.
“But back to Montreal…I went in the long vacation after second year. I’d never been on a plane and it was a great adventure. I’d also never seen a patient and that was a bit of a problem because it turned out that “second year” in Canada meant something very different to what it meant in the UK. But my hosts were very generous and wanted to persuade medical students to choose anaesthesia as a career. I spent the summer in two intensive care units, one run by the anaesthetists and the other by clinical pharmacologists. I had enjoyed pharmacology the previous year and here it was in action: I loved it and I had some great mentors encouraging me to understand more. This early experience led eventually to my choice of career. I also loved Montreal and I went back for some of my later clinical attachments, including Paediatrics.
“Medical students in North America did much more hands-on clinical work than we did and one day I was asked to carry out a procedure on a small baby that I had no experience of doing. I said that I thought I needed supervision, but was told simply to get on with it. I refused; there was a stand-off with the senior resident; I still refused and someone else did it. The incident was never mentioned again – until I got back to Oxford, where I studied, and was summoned to the Professor of Paediatrics who showed me a letter from Montreal.
“These days, I hope my stance would be viewed as good awareness of my limitations and a genuine concern for the welfare of the baby. However, much was made of my “unpleasant disagreement”, lack of professionalism, etc. I was very upset that the matter had not been raised and resolved in Montreal and disappointed that my explanation was not given more weight in Oxford: I had brought shame on the medical school, apparently.
“I had never considered a career in academic medicine anyway and planned to go back home to Cornwall to train as a GP. This experience confirmed my choice. I decided I wouldn’t even try to get a house job (FY1) in Oxford and applied to Truro – who turned me down! They told me that the consultants only appointed people from Bristol or their own medical school and no one from Oxford would be considered. Later in my career, when consultants of a certain age looked back wistfully on the “good old days” I thought of that experience. I then applied to other locations in the west country but they also turned me down and time was running out. I enquired in the medical school office and was told that the only remaining jobs were a newly established link with Stoke-on-Trent. I didn’t know where that was and had to look on a road atlas.
“Nowhere looks its best on a wet Friday afternoon in November and this was certainly true of the Potteries, but at the interview I had a warm welcome from very nice consultants and accepted the post. And then I got a letter from Oxford’s equivalent of the Dean, raising the Montreal thing again and expressing concern about what kind of ambassador I was going to be for the medical school. I kept the letter.
“In Stoke I worked for consultants who were approachable, supportive and encouraging. I began to enjoy medicine as I really hadn’t done before and, one day, my boss took me aside and said that he thought I should consider a career in academic medicine. And so my life took another turn that I had not wanted or expected but for which, looking back, I am immensely grateful.
“Move on a few decades and, as Chair of the GMC and by now with a knighthood, I was invited to give a talk to the final year medical students at Oxford. On such occasions I always emphasised that an indifferent record as a medical student needn’t have a negative impact on your subsequent career. To give this point local interest I showed the letter I had received all those years before. After the talk an elderly gentleman came down from the back: it was none other than the author of the letter! He was very gracious – and I left Oxford thinking that it’s a funny old life.”

Thank you Peter Rubin. You have inspired many of us to go on and have successful medical careers both in the UK and abroad. I fondly remember being Dr Rubin’s JHO and him telling us all that grades and failing professional exams aren’t that important, but that hard work is! The last time I saw Dr Rubin was as a Neuroradioogy fellow at about 4am with a sick patient by the CT scanner at QMC, still working hard! I’m now happily working as a radiologist in the USA and wanted to thank Dr Rubin and all my Professors and senior trainees at the University of Nottingham for a really fantastic world class training !
How lovely to hear this personal an honest story from you Peter. What a courageous person you were even in your younger days speaking truth to power. An inspiration to us all to stand up for what is right and to see bad experiences as an opportunity. Wonderful.